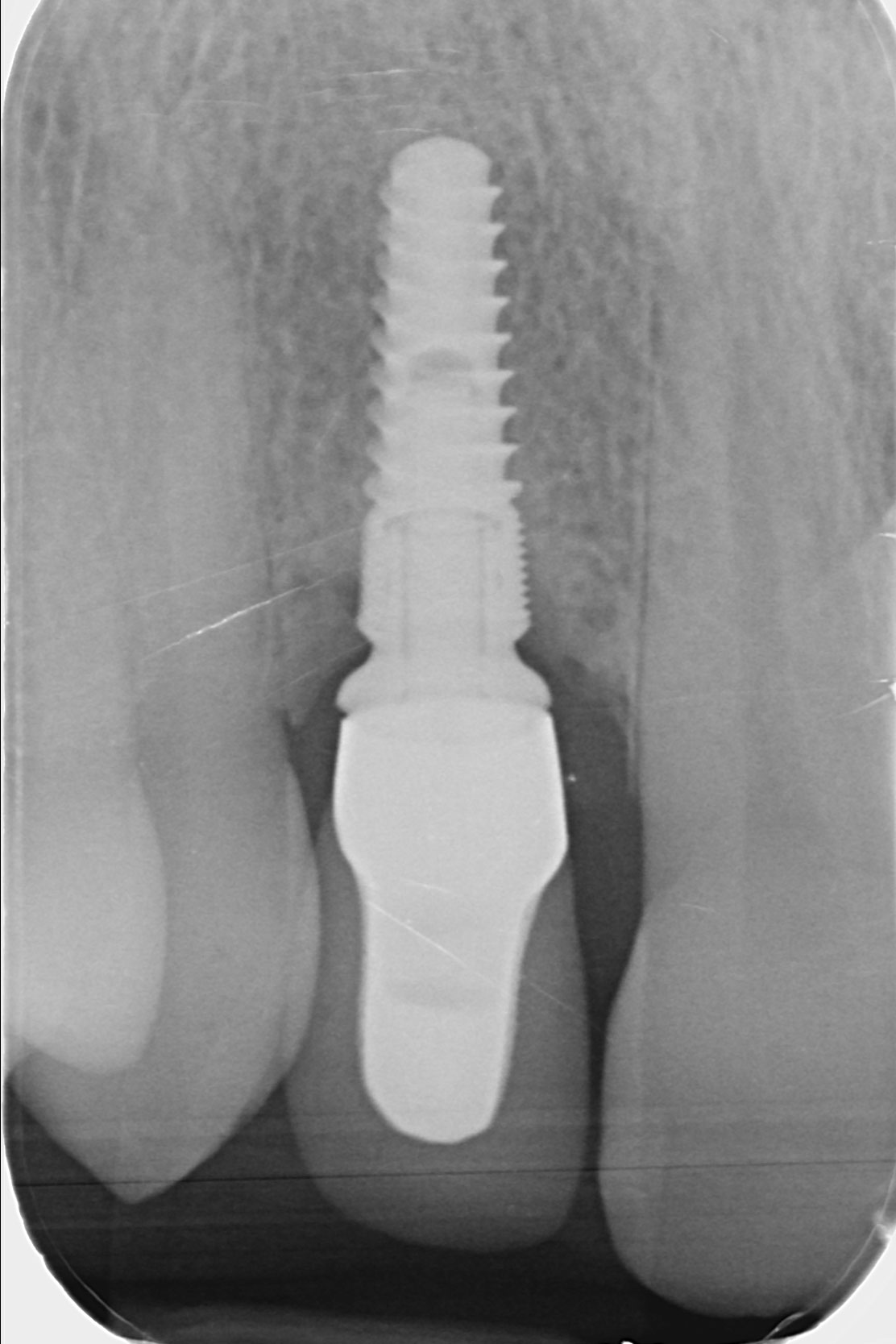
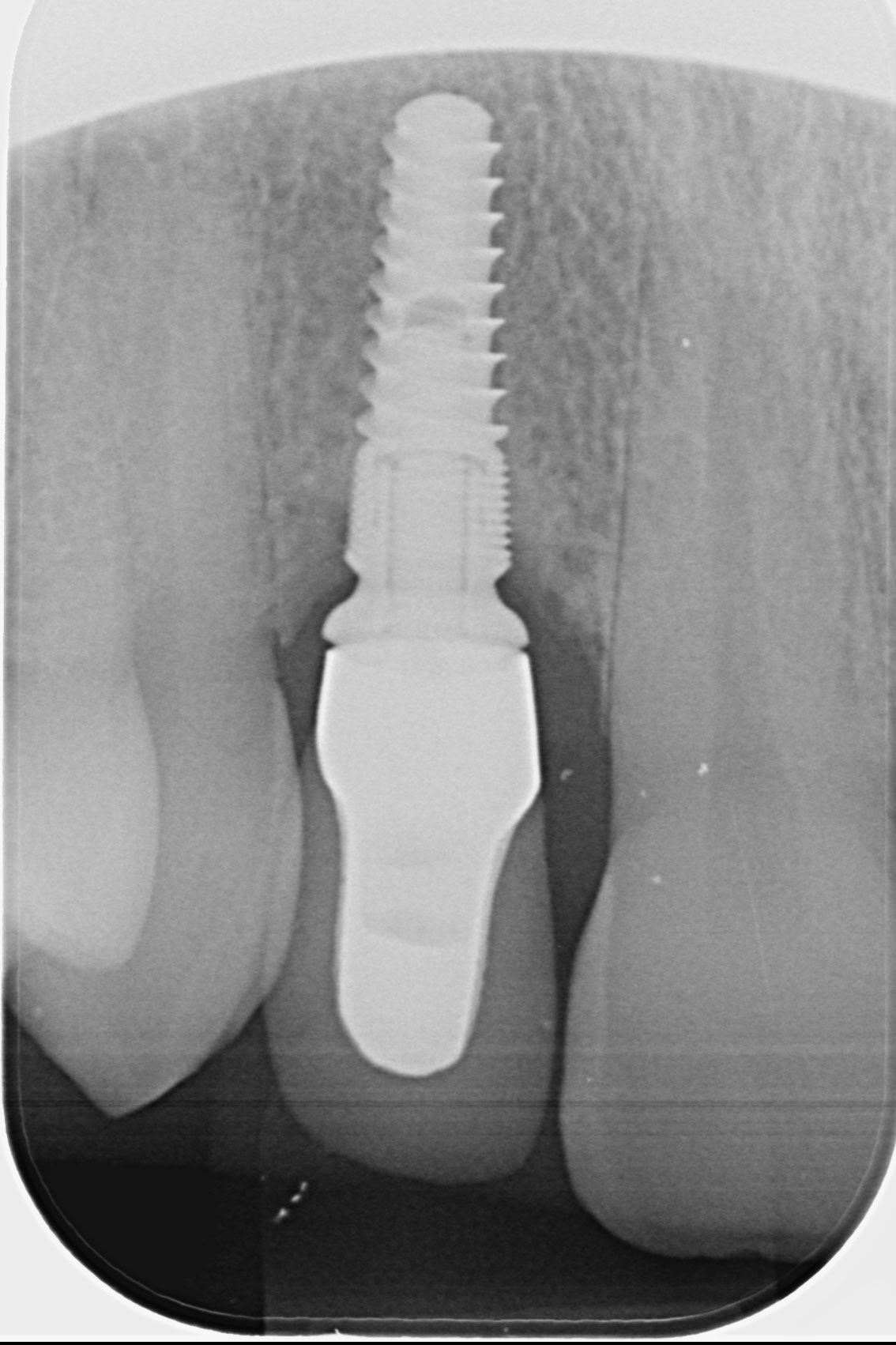
Periimplantitis surgical treatment in the esthetic area, with miniinvasive surgery and tissue reconstruction.
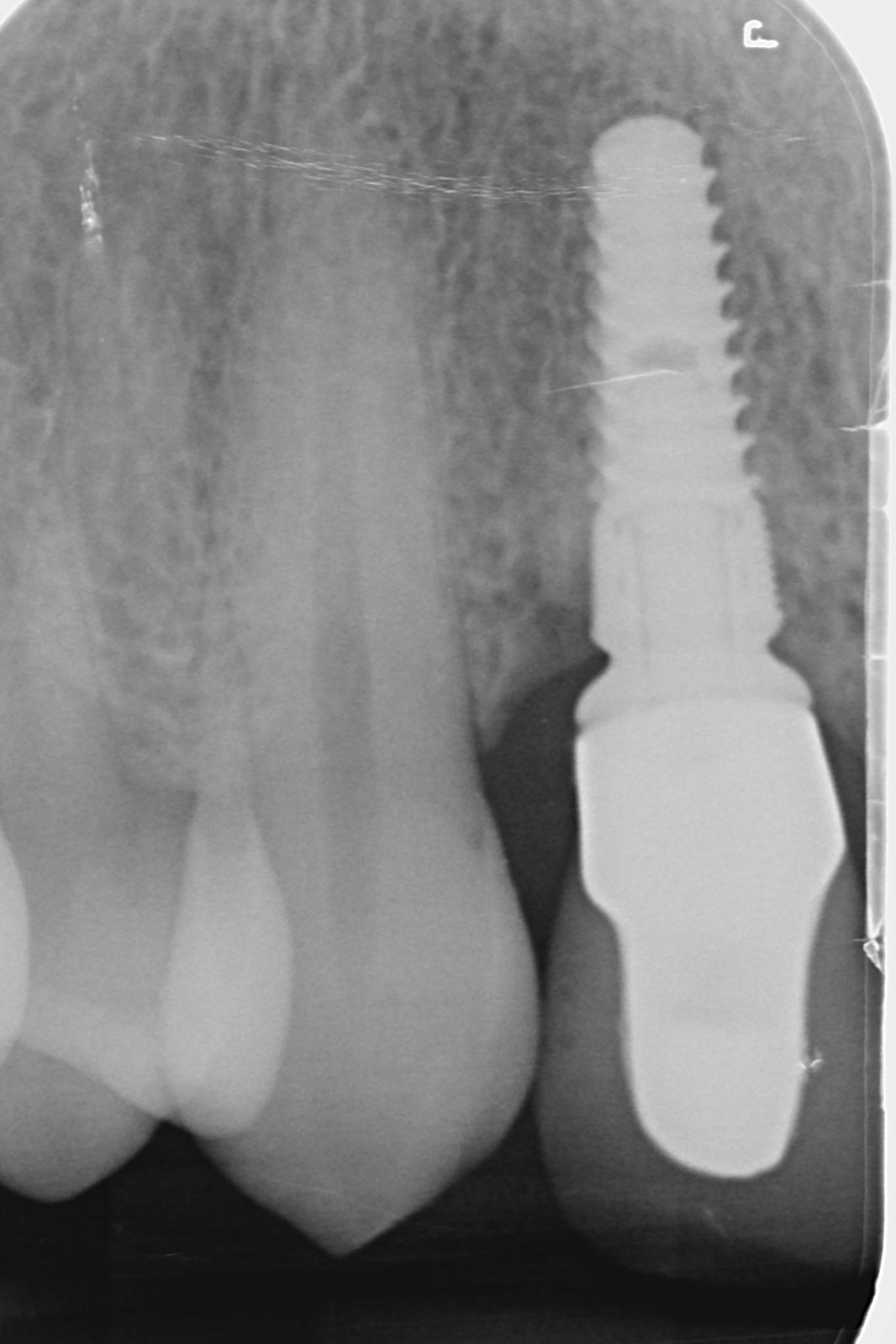
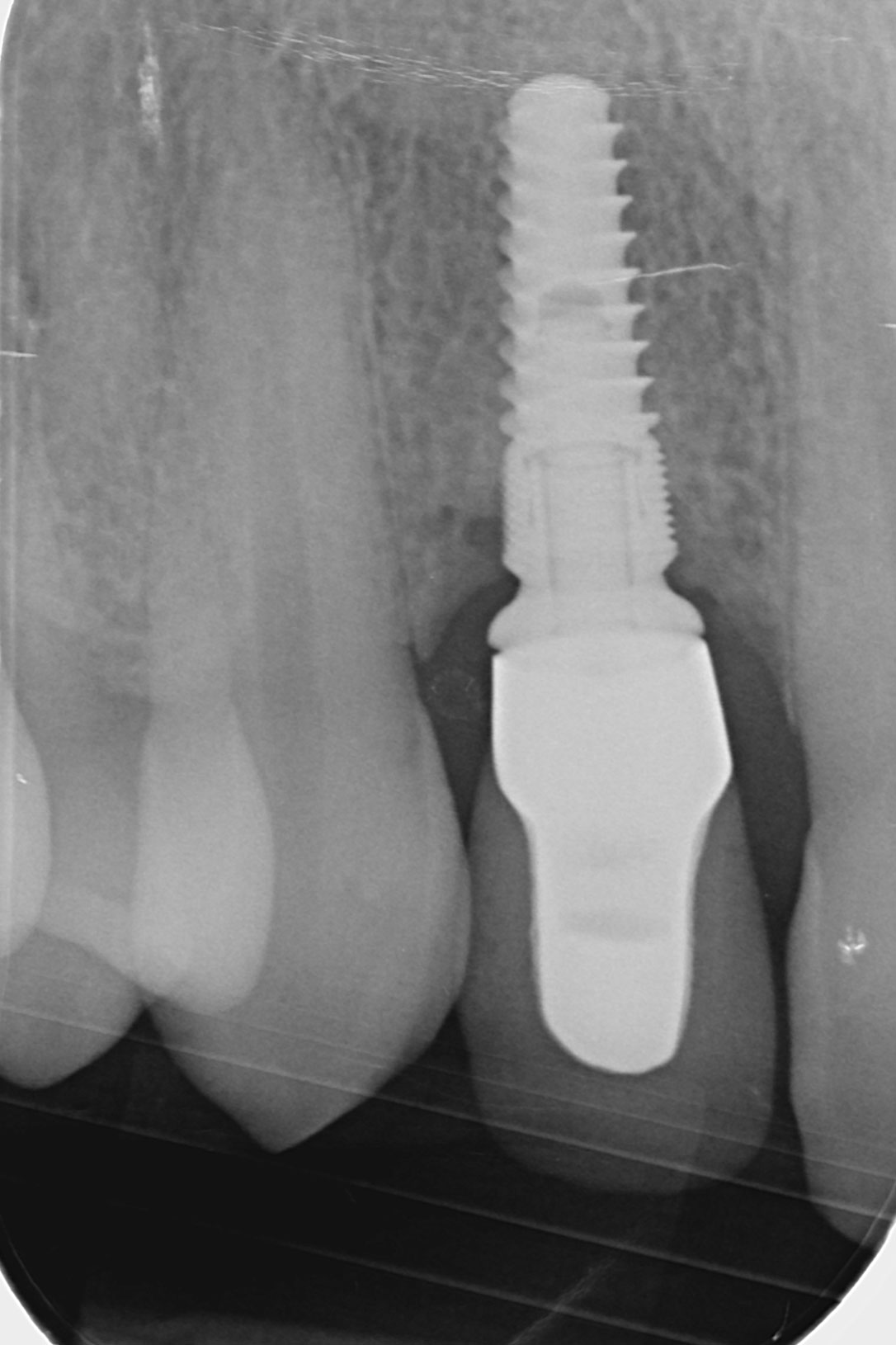
Peri-implantitis is a plaque-induced pathology of peri-implant tissues, characterized by inflammation of the peri-implant mucosa and subsequent progressive loss of the bone support. The diagnosis of peri-implantitis is based on the following signs:
- presence of bleeding and/or suppuration on probing
- probing depth ≥ 6 mm
- peri-implant bone level located more than 3 mm apical to the most coronal portion of the intraosseous coronal portion of the implant [1]
The treatment of periimplantitis includes control of the etiological factors, decontamination of the implant surface and, if necessary, reconstruction of the periimplant tissues (bone and soft tissue) [2] There is still no consensus on the surgical approach for the treatment of peri-implantitis.
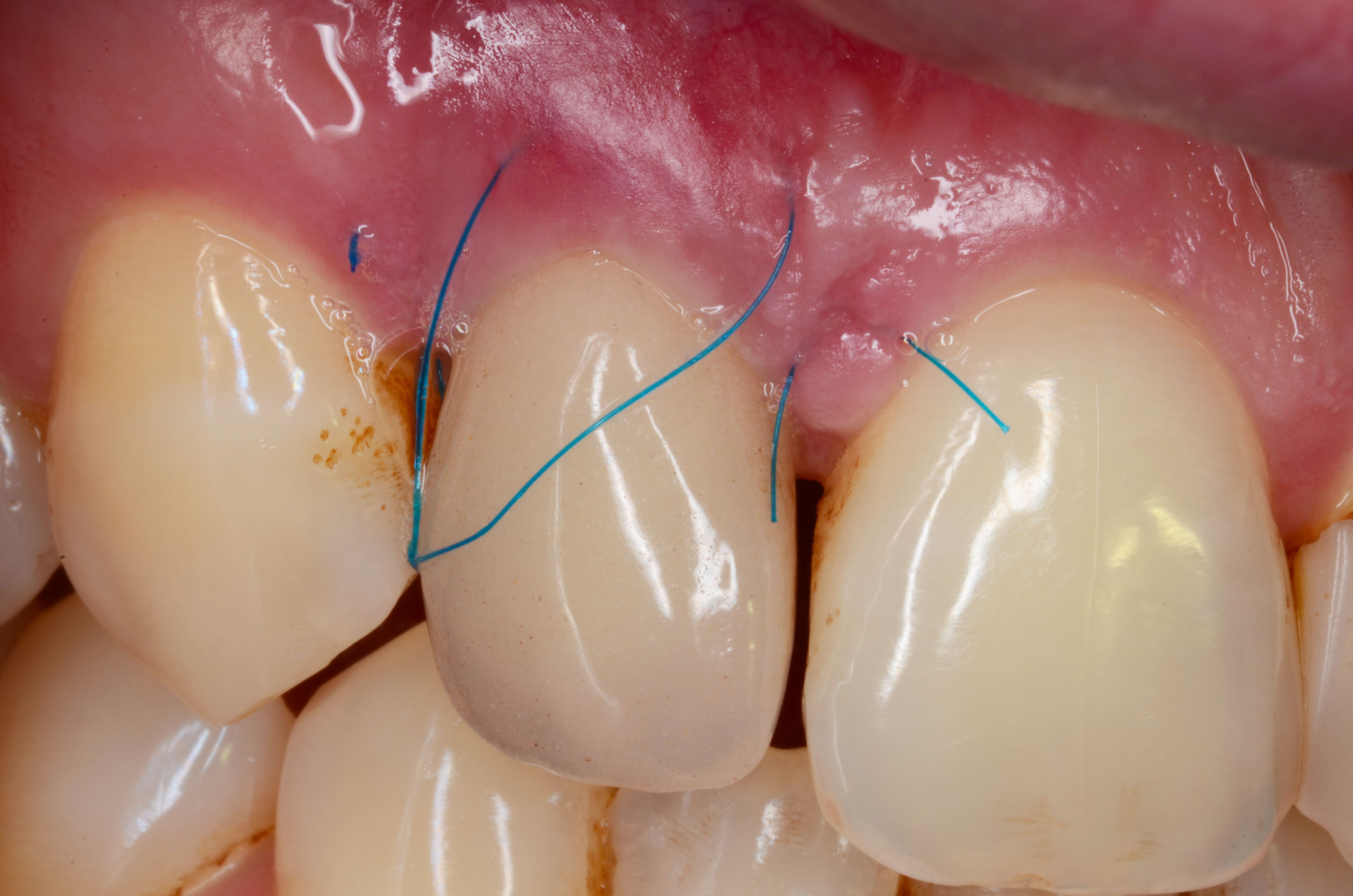
As thin biotypes are associated with more soft tissue recession around implants, a sufficient thickness of soft tissue is recommended, especially in the aesthetic area [3]. This clinical case takes into account the etiology, the treatment proposals and the risk factors.


The proposed treatment plan is:
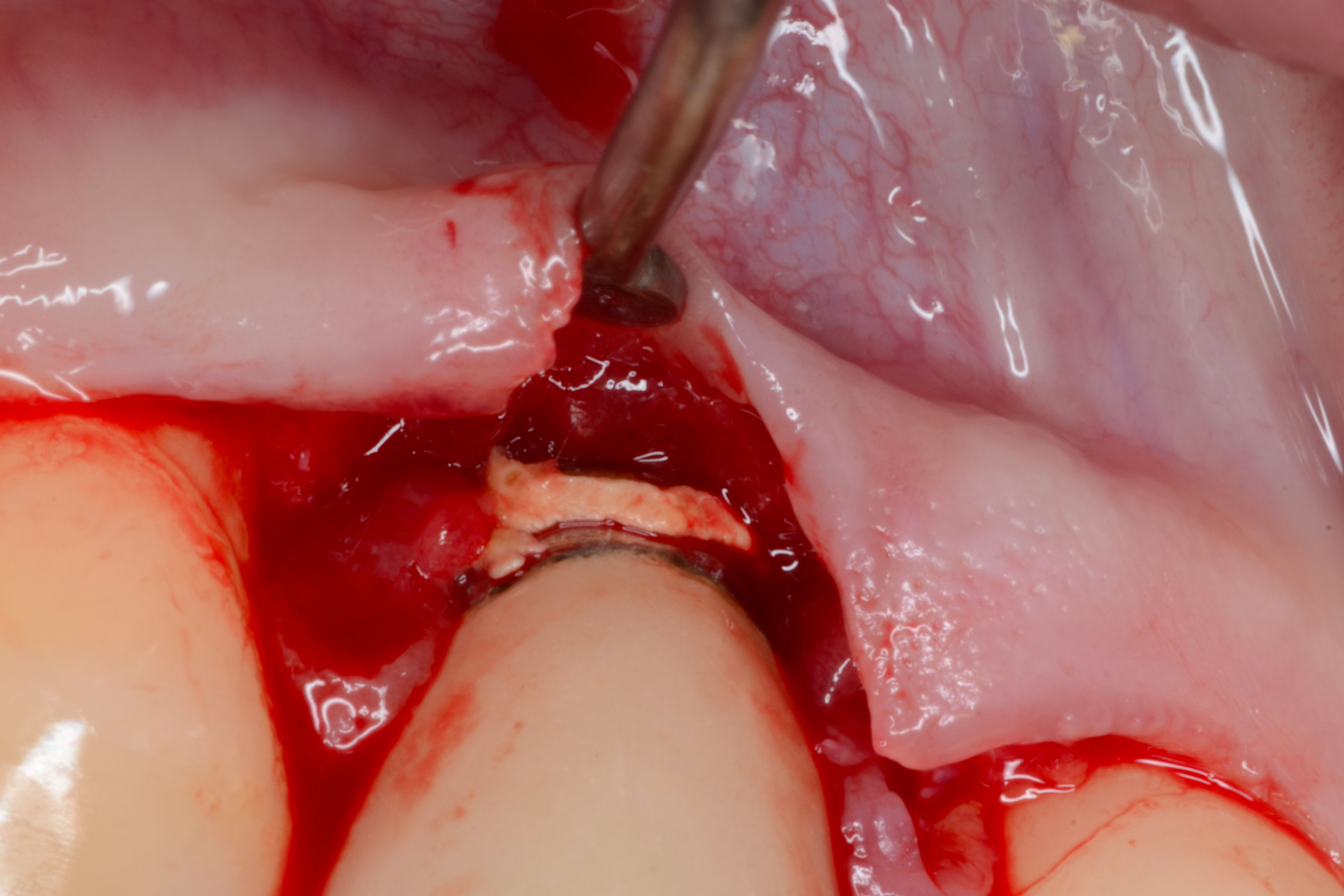
- Initial therapy (inflammation control) : oral hygiene and global scaling and polishing
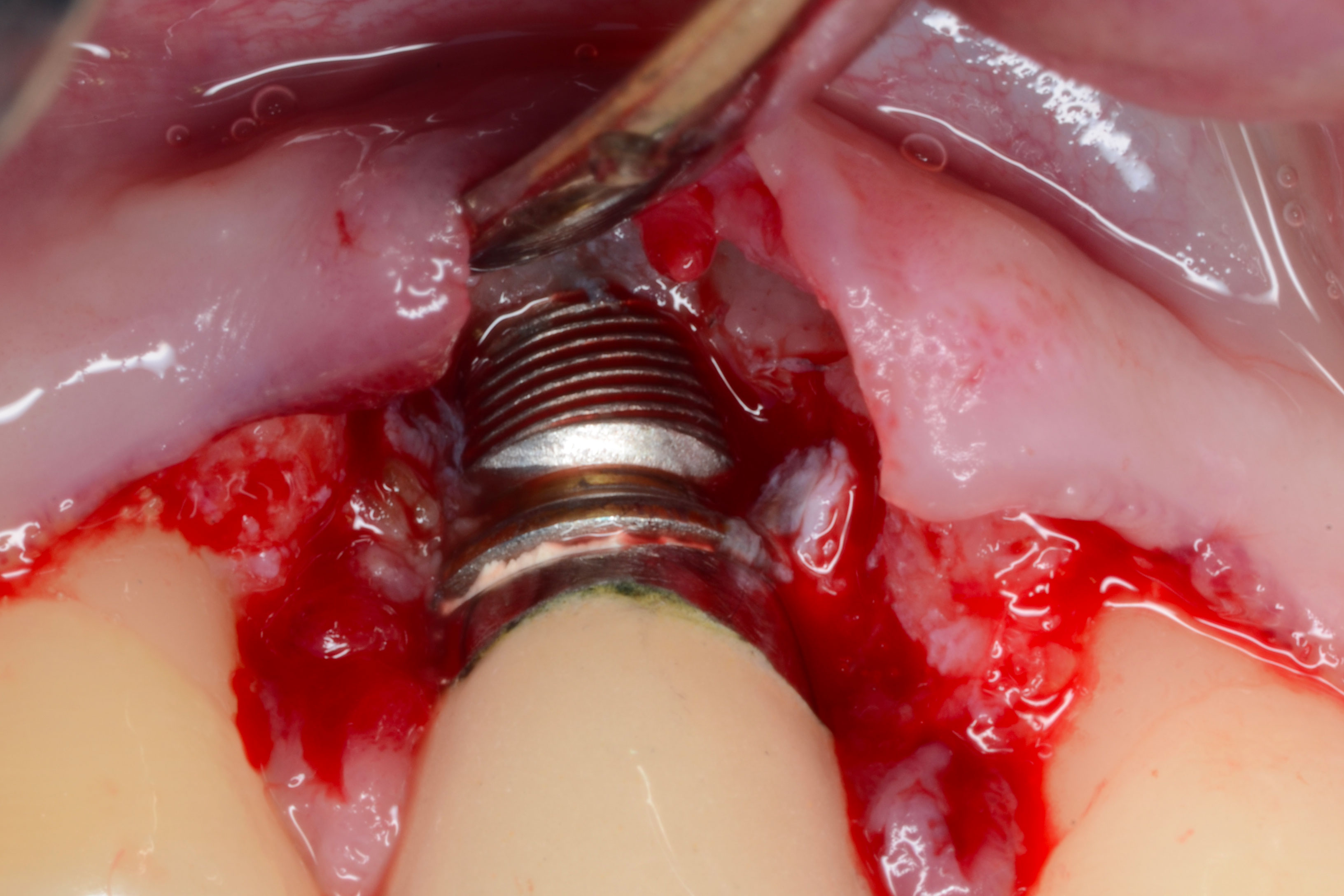
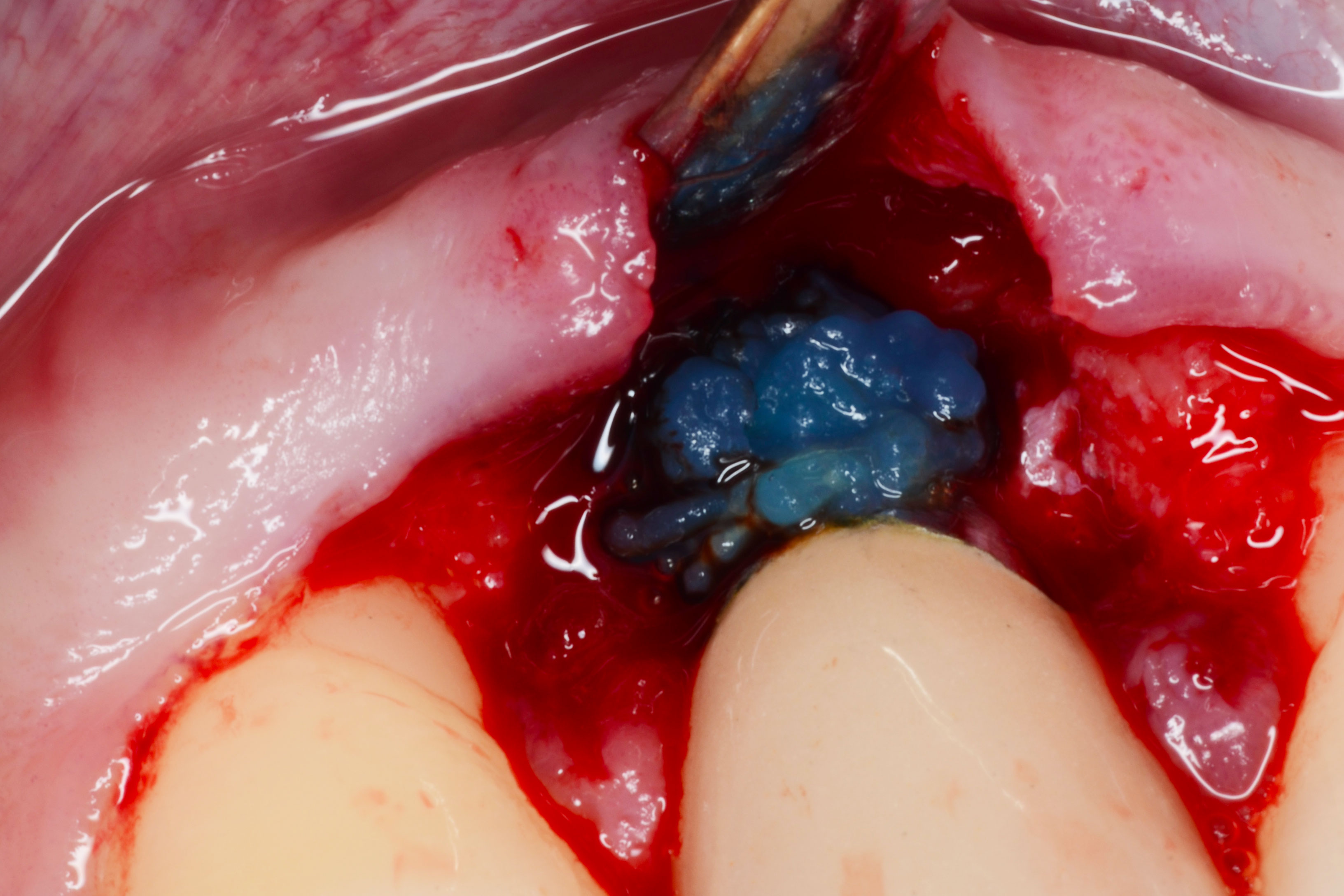
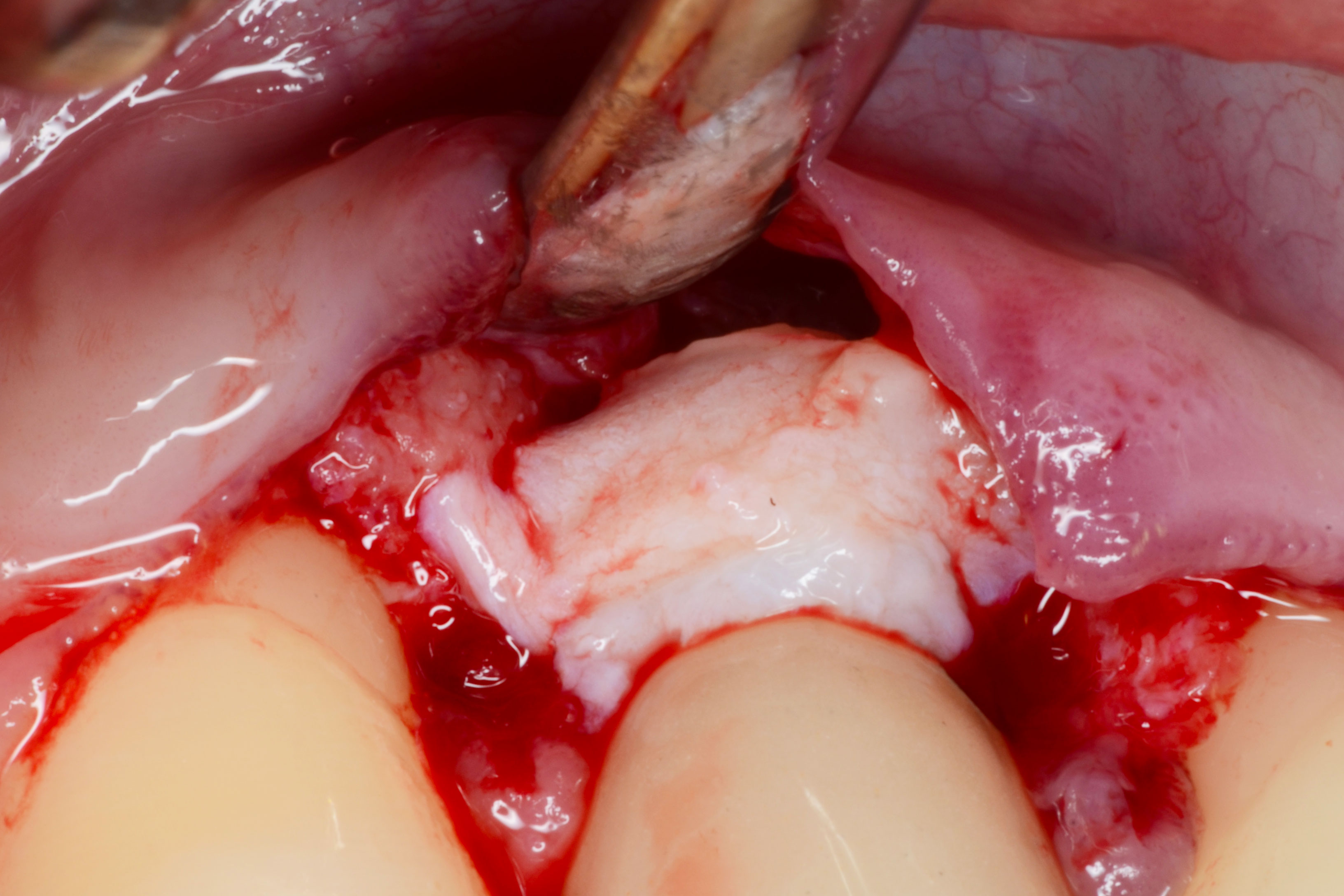
- Mini-invasive surgery: bony lesion curetage, implant decontamination
- Bone reconstruction if necessary
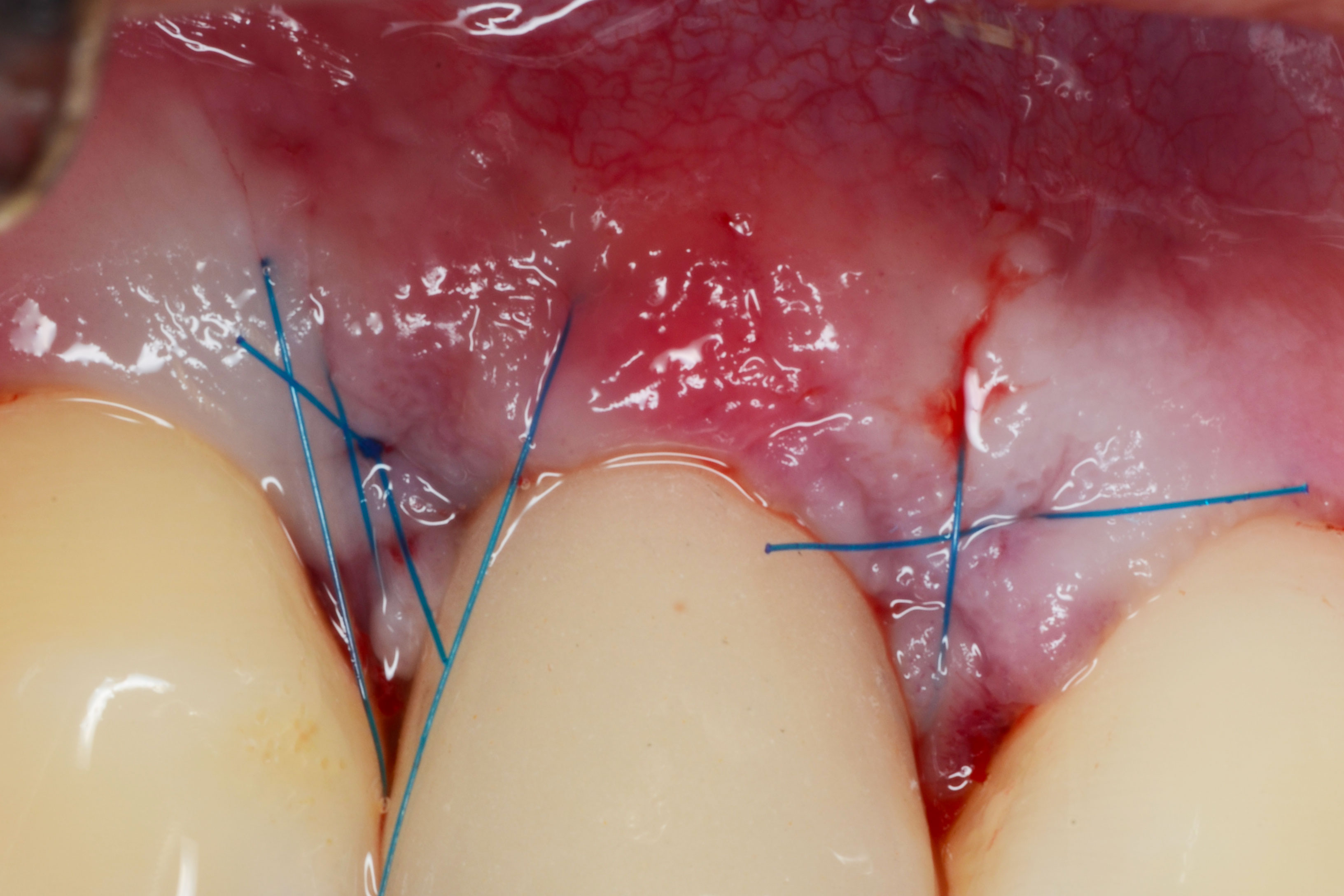
- Soft tissue reconstruction (connective tissue graft)
- Periodontal supportive therapy




References
- Berglundh, T., et al., Peri-implant diseases and conditions: Consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Clin Periodontol, 2018. 45 Suppl 20: p. S286-S291.
- Berglundh, T., J.L. Wennstrom, and J. Lindhe, Long-term outcome of surgical treatment of peri-implantitis. A 2-11-year retrospective study. Clin Oral Implants Res, 2018. 29(4): p. 404-410.
- Chackartchi, T., G.E. Romanos, and A. Sculean, Soft tissue-related complications and management around dental implants. Periodontol 2000, 2019. 81(1): p. 124-138.
- Staubli, N., et al., Excess cement and the risk of peri-implant disease - a systematic review. Clin Oral Implants Res, 2017. 28(10): p. 1278-1290.

